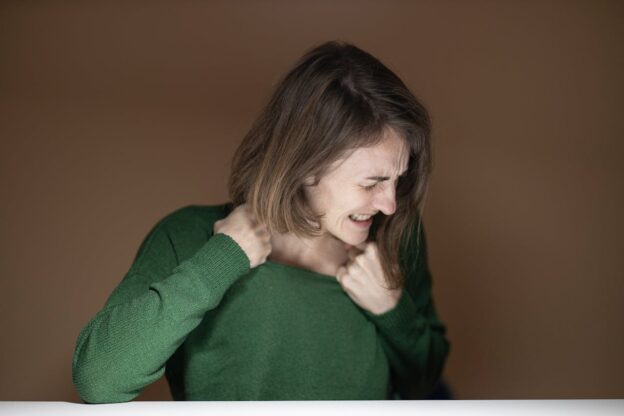
Quitting alcohol is a major win, but sometimes, things still feel off. You’re sober, but you might feel stuck, angry, or like something’s missing. That’s often a sign of dry drunk syndrome. It happens when someone stops drinking but doesn’t feel better emotionally. If you relate to this, you’re not alone. These struggles are more common than people think, and they don’t mean you’ve failed. Many people experience this stage in recovery. It just means you may need more support. Some drug and alcohol treatment centers in West Virginia understand how this feels and know how to help. You deserve support that actually helps you grow—emotionally and mentally.