Tricare Insurance For Substance Abuse Treatment Coverage
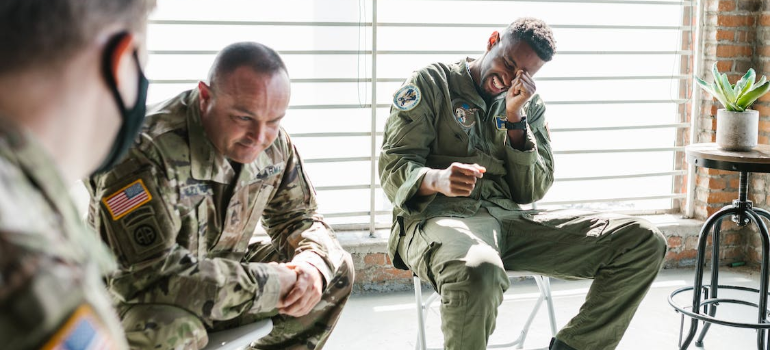
At Harmony Ridge Recovery Center, we are honored to work with Tricare and provide comprehensive support for military members, veterans, and their families.
The rehabilitation process can be incredibly challenging all on its own before considering costs. Making that first step forward requires courage, and the prospect of going through the process may be stressful enough already. With that in mind, the last thing you need as you embark on a journey to recovery is confusion over expenses and your plan’s coverage. If you’re reading this article, you’re likely looking for drug rehab that accepts TRICARE – clearly and with no complicated jargon.
With Harmony Ridge Recovery, you don’t have to worry about murky waters, hidden fees, plan ineligibility, and so on. From the very first steps of admission, we will explore your financing options together and craft a clear and concise plan that works for you. In addition, we accept TRICARE – one of the most prominent health insurance providers in the US today.
Payment Plans and Insurances Coverage at Harmony Ridge
First and foremost, we should clarify that we accept all major insurance providers, including:
- Humana Insurance
- Blue Cross Blue Shield
- TRICARE Insurance
- PEIA Insurance
However, not all providers and plans will cover the full expenses of your treatment. Factors like the following will affect your final coverage:
- Prior addiction history
- Treatment duration and needs
- Exact services received
- Other state-side factors
As such, it would be irresponsible to simply claim your programs will be covered in full at all times. Instead, we must refer you to our representatives, who will explore your plan and suggest alternatives as needed. Please contact our teams at (855) 942-3797 for a full review of your financial options.

Things You Should Know About TRICARE Insurance Plan
TRICARE is a rather unique type of insurance provider. In brief, it primarily caters to active military personnel, military retirees, and their dependents, making it a common plan to cover rehab for veterans. TRICARE is part of the Defense Health Agency (DHA), a component of the Military Health System.
In turn, it may differ drastically from other insurance plans in terms of eligibility and more. To cover these distinguishing factors, as a center for drug rehab that accepts TRICARE, here we may thoroughly cover the fundamentals of TRICARE.
The History of TRICARE
The foundations for TRICARE were laid with the Civilian Health and Medical Program of the United States (CHAMPUS) in the mid-1960s. Trying times, with the Vietnam War underway, had the Department of Defense (DOD) take measures to ensure proper healthcare for the military. The Military Officers Association of America (MOAA) relays the events as follows:
“The population of military retirees and dependents ballooned, straining a health system that previously could accommodate most beneficiaries at military facilities or sent family members to private facilities for inpatient care.
To ensure that the booming population of retirees and family members assigned to locations not near a base had access to health services, Congress created CHAMPUS, a fee-for-service insurance plan requiring cost shares but without the premiums or enrollment fees of traditional insurance.”
In the years that followed, TRICARE saw immense popularity, which strained the DOD’s budget. Beneficiaries skyrocketed as well, with MOAA quantifying the increase at 162% during the decade between 1981 and 1990 alone. Simultaneously, nationwide healthcare reforms in the ‘80s and the emergence of health maintenance organizations (HMOs) cemented TRICARE’s future form.

TRICARE was thus formally born in the 1990s, as Congress saw a solution for CHAMPUS in the HMO model. It began with six healthcare contractors who would manage beneficiaries in 12 regions, overseen by the TRICARE Management Activity body. In this form, it included 3 programs:
- TRICARE Prime, which most closely followed the HMO model
- TRICARE Extra, which incentivized beneficiaries to choose civilian providers within its network
- TRICARE Standard, which resembled the initial CHAMPUS form and allowed non-network provider visits at extra cost
Today, TRICARE offers 11 distinct plans. Any drug rehab that accepts TRICARE will, unless otherwise noted, accept all such plans and use them to finance your treatment in part or in full.
Eligibility
In its current form, eligibility for TRICARE is reserved for the following:
- Uniformed Service members and their families
- National Guard/Reserve members and their families,
- Survivors,
- Former spouses,
- Medal of Honor recipients and their families, and
- Others registered in the Defense Enrollment Eligibility Reporting System (DEERS).
National Guard/Reserve members can include members of the:
- Army National Guard
- Army Reserve
- Navy Reserve
- Marine Corps Reserve
- Air National Guard
- Air Force Reserve
- S. Coast Guard Reserve
In addition, TRICARE specifies two types of beneficiaries:
- Sponsors, who are active duty, retired, and Guard/Reserve members, and
- Family members who are spouses and children who are registered in DEERS.
These are all notable because benefits and plans do vary depending on one’s beneficiary category and other factors.
For complete information on eligibility, we strongly encourage you to visit TRICARE’s website linked above. For additional information on their programs and their respective history, you may also visit the Health Insurance Glossary page that the Centers for Disease Control and Prevention (CDC) offer.

Understanding The Terms
On the subject of glossaries, however, healthcare can be quite frustrating as regards terms and terminology. Not all such terms exist in everyday discourse, and those which don’t often carry the same meaning. So, here we may outline the 12 most crucial terms you should know before seeking drug rehab that accepts TRICARE.
#1 Network provider
One of the most fundamental terms for any plan, a network provider is any healthcare provider under contract with TRICARE regional contractors. Thankfully, TRICARE offers a handy tool to help you find a doctor who is part of the network.
#2 Non-network provider
In contrast, non-network providers are healthcare providers who are not within the network. A distinction to make here is that these providers come in two types:
- These providers will accept payment directly from TRICARE, despite not being part of the network, and have agreed to the charge rates of TRICARE as full payment. They will choose to participate on a case-by-case basis.
- Non-participating. These providers will not file your claims, meaning you will often have to pay upfront and do so yourself. They’re legally allowed to charge up to 15% above TRICARE’s charge rates, and the difference will be on you to cover.
#3 Primary care manager
A term exclusive to plans like TRICARE Prime, it refers to a healthcare provider who will serve as the primary provider and coordinator for healthcare services you receive. Primary Care Managers (PCMs) can be providers within the network, whether they’re employed in military hospitals, civilian clinics, or under the US Family Health Plan.

#4 Referral
A strict responsibility of your PCM, a referral is when your PCM refers you to other providers for healthcare services. If this is not an option, you will need to opt for the point-of-service (POS) option, where you’ll pay more out of pocket. Notably, referrals are not a requirement of some TRICARE plans, such as TRICARE Select.
#5 Enrollment fee
Unlike other applications of the term, here, the enrollment fee refers to the annual amount you may need to pay for your healthcare coverage. This is not necessary across the board, as some beneficiaries do not pay enrollment fees – most notably active duty service members and their immediate families. Other plans may also not have any enrollment fees.
#6 Annual deductible
Like in its colloquial uses, the annual deductible is the amount one pays before their plan initiates cost-sharing. Like other fees discussed below, it resets every year.
The plans which have annual deductibles are:
- TRICARE Select
- TRICARE Overseas Program Select
- TRICARE Reserve Select
- TRICARE Retired Reserve
- TRICARE Young Adult Select
Other deductibles may exist depending on your plan and Medicare coverage.
#7 Cost-share
In turn, cost-sharing refers to the percentage of your received services’ cost you pay after meeting your annual deductible. This, too, may vary across plans and depending on the providers and types of care you receive.
Notably, cost-shares do not apply to active duty service members. This is crucial for any drug rehab that accepts TRICARE to note as well.
#8 Copayment
Unlike cost-shares, copayment refers to a fixed amount beneficiaries pay for services their plan covers. Copayments also vary depending on an array of factors, such as your plan, beneficiary type, and more.
Just like cost-sharing, active duty service members do not pay for any out-of-pocket costs. Their family members also have no copayments if they’re covered by TRICARE Prime specifically.

#9 Premium
A simpler term, a premium is the amount you pay to maintain your healthcare coverage under TRICARE. The plans which have premiums are:
- TRICARE Reserve Select (monthly)
- TRICARE Retired Reserve (monthly)
- TRICARE Young Adult (monthly)
- Continued Health Care Benefit Program (quarterly)
#10 Catastrophic cap
As the name suggests, the catastrophic cap refers to the maximum amount you may pay each year for services covered by your plan. This, too, resets every year and includes:
- Enrollment fees
- Deductibles
- Copayments
- Cost-shares
The two exceptions of costs that don’t count toward your catastrophic cap are:
- Premiums for premium-based plans, and
- Point-of-service (POS) fees for TRICARE Prime
#11 Medically necessary
A crucial term for both beneficiaries and any drug rehab that accepts TRICARE, “medically necessary” is a qualification for any healthcare services received. This is a very strict set of criteria applied by medical professions, which holds that all healthcare services and supplies received must be:
- Appropriate
- Reasonable
- Adequate for your condition’s diagnosis and treatment
In addition, all such services must also be demonstrably safe and effective, as proved by rigid scientific criteria.
#12 Other Health Insurance
Finally, Other Health Insurance (OHI) refers to any other health insurance you may have other than TRICARE. This term is crucial to note as well, as TRICARE pays after most OHI, with very few exceptions. By law, these exceptions are:
- Medicaid
- TRICARE supplements
- State Victims of Crime Compensation programs
- Federal government programs
In such cases, you should inform your provider of your OHI and file your claims in order.

If you need additional information on TRICARE’s terms specifically, they thankfully also offer resources you may explore. Among them, you may consider the following:
- TRICARE’s cost terms page
- Their newsroom article on healthcare terms
- Their newsroom article on healthcare costs-related terms
Wide Plethora of Recovery Programs You Can Choose From
Being a center for drug rehab that accepts TRICARE may not suffice to meet your needs – beyond the financial ones. As such, we at Harmony Ridge offer an array of recovery programs to suit each and every rehabilitation.
Our 4 primary programs after medical detox, in order, are the following.
Residential Program
A type of Inpatient program, our residential program offers safe and welcoming designated facilities for our patients. It typically caters to the cases which require the most intensive care, as it is the most appropriate program following medication-assisted detox (MAT).
It offers 24-hour medical supervision, a keen focus on clinical services and psychiatric care where needed, and strict case management as it sets the foundations for aftercare. Driven by our qualified, experienced medical staff and expert therapists, Harmony Ridge is the residential treatment center West Virginia trusts.
Intensive Outpatient Program (IOP)
Following Inpatient programs or PHPs, or also as standalone steps, come Outpatient programs. Such programs allow patients to reside at home and seek therapy in their rehab centers for specific hours each week.
On this front, we offer a variant the industry calls the Intensive Outpatient Program (IOP). Unlike its common variant, our IOP requires more hours of therapy to help address the underlying causes of addiction. It employs an array of therapeutic techniques, continues to build relapse prevention tools for aftercare, and allows the individual to vocalize their challenges to their peers in group therapy settings. If you need an IOP to best meet your case’s needs, look no further than the intensive outpatient program West Virginia trusts at Harmony Ridge.
The Difference Between Inpatient and Outpatient Program - Find The Best Option for you
All that said, we understand such terms are similar to health insurance terms, rare in common language, and perhaps confusing. With this in mind, here we may consolidate the key differences between Inpatient and Outpatient programs. In doing so, we’ll hopefully help you weigh your options and find the one that best suits you.
In brief, the two differ in 3 key regards, which are as follows.
#1 Residence
Inpatient programs require that you live in designated facilities for their duration so that you’re removed from harmful distractions and under close medical supervision. In contrast, Outpatient programs cater to comparatively milder cases, so they allow you to stay at home for their duration. This has the benefit of schedule lenience, which may allow you to see to other duties you may have.

#2 Intensity
As regards the intensity of care, Inpatient programs are much more intense than Outpatient programs. They both offer various types of therapy, but Inpatient programs will require more hours of therapy and more strict supervision. In contrast, Outpatient programs tend to be much more lenient, especially if they’re not IOPs.
#3 Therapy focus
Finally, each of the two will primarily focus on different types of therapy. Inpatient programs will focus more heavily on withdrawal symptom management, pharmacotherapy, individual therapy, and psychiatric care if needed. Outpatient programs, on the other hand, will focus more on cognitive and behavioral therapy alongside group and family therapy.
All Addictions Are Curable
Still, regardless of the program that best suits you, here we must reassure you that indeed, all addictions are curable. If you’re looking for drug rehab that accepts TRICARE, chances are you fear that your addiction may not be. However, our experience has shown that, while each addiction does differ, all addictions can be treated with proper care – and our catalog reflects that experience.
At Harmony Ridge, we treat the following addiction types.
Alcohol
An increasingly common type of addiction, alcohol misuse can quickly escalate into dependency and endanger the individual. From 12-step programs to more options, we offer extensive services for alcohol rehab WV prefers.
Cocaine
An illicit substance and a powerful stimulant, cocaine is both highly addictive and very destructive. Whether it’s for you or your loved ones, our cocaine addiction rehab center comes fully equipped to uproot any addiction to cocaine.
Fentanyl
Fentanyl is a synthetic opioid with notable uses as a painkiller. However, prolonged use and misuse for non-medical purposes can quickly develop into an addiction – for which we offer extensive fentanyl detox treatment services.
Heroin
An infamous illicit drug, heroin is a highly addictive substance with notable overdose rates. It may not fuel as many addictions as it used to, as our heroin rehab centers will attest to, but heroin remains a very dangerous substance.

Meth
Another stimulant, better known as “meth”, this drug medically goes by “Methamphetamine.” It is among the most commonly used illicit drugs today, as well as one of the most highly addictive ones. If you’re looking for a meth rehab center West Virginia has to offer, look no further than Harmony Ridge.
Ambien
Approved by the FDA to treat insomnia and similar sleeping disorders, Ambien remains highly addictive over prolonged use or if misused. For this reason, we also offer extensive Ambien rehab services.
Barbiturates
A type of depressants, barbiturates can also be used medically to treat sleeping disorders. Over the years, they have consistently proved to be quite addictive as well, making barbiturates rehab services a need we are proud to cater to.
Benzodiazepine
Better known as “benzo”, Benzodiazepine is another type of depressants. Much like the other medical drugs on this list, benzos can commonly fuel addiction. If you or your loved ones need benzo rehab, we at Harmony Ridge offer such services as well.
Stimulants
A drug type in itself, stimulants come in both illicit varieties, such as cocaine, and medical ones, like Adderall, Ritalin, Concerta, and others. Their medical use as a treatment for ADD and similar disorders aside, stimulants also see misuse and can be highly addictive. To address this, our stimulants addiction rehab center comes fully equipped for this type of addiction as well.
Opiates
Opiates are a subcategory of opioids, and today they spearhead the nationwide opioid epidemic. Our opiate rehab center takes this health crisis seriously and comes prepared to treat this type of addiction with utmost care.
Marijuana

Legal in some states due to its many medical uses, marijuana still sees misuse as an illicit recreational drug. While it does not typically endanger the individual as much as other drugs, marijuana addiction remains a task our marijuana rehab center is prepared to handle.
The Admission Process - how to get started?
With all of the above in mind, our offerings and perks over our peers should now be clear. We are not just a center for drug rehab that accepts TRICARE, but we also come equipped to treat an array of addictions through a variety of programs. Still, if you’ve made up your mind, you may still not know where to begin.
Thankfully, our admission process is as simple as it is discreet and considerate. You will only need to get in contact with our admissions agents, either by filling out our admission form or contacting us directly at (855) 942-3797.

Once you do, we will go over your unique case and make appropriate recommendations for programs and therapies. We will review your insurance plan, calculate final costs, and explore additional financing options if your plan does not cover the entirety of your program. Finally, we will answer any additional questions you might have so that you have the peace of mind you deserve before embarking on your journey to recovery.
FAQ
Does Tricare Insurance Cover Mental Health Treatment?
Tricare insurance covers mental health treatment. When treating addiction, it’s crucial to take into account the underlying roots of addiction. It is much more than a physical disease. Addiction affects an individual’s emotional and mental state as well.
Fortunately, with Tricare insurance, you’ll be able to reap the benefits of mental health treatment at our recovery center. We offer many evidence-based forms of therapy, such as cognitive behavioral therapy and group therapy.
Therapy will help you develop a toolkit of skills that will help you cope with stress and cravings. Each recovering individual will receive a unique combination of services that best suits their recovery needs.
What Are Co-Occurring Disorders?
Co-occurring disorders are when an individual has an addiction as well as a mental illness. These are treated at our recovery center. If you require treatment for a mental health disorder and addiction, then you’ll require dual diagnosis treatment.
Dual diagnosis treatment targets co-occurring disorders through different methods. We treat disorders such as:
- Anxiety
- Depression
- Eating disorders
- Bipolar disorder
- Post-traumatic stress disorder
How Do We Determine Your Benefits?
When we go through Tricare insurance, we’ll be able to let you know exactly what your plan offers. Our goal is to provide you with the highest quality of treatment at the most effective cost. Our dedicated addiction treatment staff will constant your Tricare insurance provider and go through your plan.
We go through a simple two-step process. The steps are as follows:
Step 1: Confirming Your Tricare Insurance Benefits
We’ll start with a complimentary and thorough evaluation of your insurance benefits. This takes a lot of stress off of your hands! We’ll reach out to your provider and determine what kind of benefits are covered under your specific plan.
Step 2: Verifying Addiction And Dual-Diagnosis Benefits Of Your Tricare Insurance Plan
After the in-depth evaluation, we’ll let you know:
- How much of the expenses your insurance company will cover
- What level of care you’ll be covered for
- The length of time you’ll be covered for inpatient care (30, 60, 90 days, etc.)
- How much you can expect to pay out-of-pocket for a treatment program
How Does Tricare Insurance Work?
You have an assigned primary care manager (PCM) who will help guide you through coverage. Your primary care manager will help:
- Refer you to specialists for the care he or she can’t provide
- Work with your regional contractor for referrals/authorization
- Accept your copayment
- Files claims for you
What Is Tricare Prime Plan?
Tricare Prime is a managed care option available in “Prime Service Areas,” such as the East Coast. This plan ensures medical readiness for active duty by adding to the capability and capacity of military hospitals and clinics. Prime Service Areas were also built around the Base Realignment and Closure sites.
Additional Prime Options for Active Duty Service Members And Their Families Include:
- Tricare Prime Remote
- Tricare Prime Overseas
- Tricare Prime Remote Overseas
Who Can Enroll In Tricare Insurance Prime?
- Active duty service members and their families
- Retired service members and their families*
- Activated
- Called or ordered to active duty service for more than 30 days in a row
- Guard/Reserve members and their families
- Non-activated Guard/Reserve members and their families who qualify for care under the Transitional Assistance Management Program
- Retired Guard/Reserve members at age 60 and their families*
- Survivors
- Medal of Honor recipients and their families
- Qualified former spouses
*When retired service members and their families become eligible for Medicare based on age, they aren’t able to participate in Tricare Prime.
How Do I Enroll In Tricare Prime?
- Online via the Beneficiary Web Enrollment website
- Call your regional contractor
- East Region: Under the new regional contracts, the East Region is a merger of the North and South Regions and includes Alabama, Arkansas, Connecticut, Delaware, the District of Columbia, Florida, Georgia, Illinois, Indiana, Iowa (Rock Island area), Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Mississippi, Missouri (St. Louis area), New Hampshire, New Jersey, New York, North Carolina, Ohio, Oklahoma, Pennsylvania, Rhode Island, South Carolina, Tennessee, Texas (excluding El Paso area), Vermont, Virginia, West Virginia, and Wisconsin. Tel: (800) 444-5445
- West Region: Alaska, Arizona, California, Colorado, Hawaii, Idaho, Iowa (excludes Rock Island arsenal area), Kansas, Minnesota, Missouri (except St. Louis area), Montana, Nebraska, Nevada, New Mexico, North Dakota, Oregon, South Dakota, Texas (southwestern corner including El Paso), Utah, Washington, and Wyoming. Tel: (844) 866-9378
- Mail the enrollment form to your regional contractor (mailing addresses on the form):
- East Region Form
- West Region Form
What Do You Pay?
Active duty service members pay nothing out-of-pocket. Active duty family members also pay nothing out-of-pocket unless using the point-of-service option.
All other members pay annual enrollment fees and network copayments.
Contact Harmony Ridge Today!
The first step toward achieving recovery is to reach out to one of the rehabs in WV that can get you on the track to recovery. Our admissions team is available 24 hours a day, 7 days a week, 365 days a year. Give us a call today!
Contact Us TodaySeek Help With Harmony Ridge Today!
Drug rehab may seem daunting and scary, and the first step is always the hardest. In all our years of experience in the field of addiction treatment, we have very often found this to be the case. Nonetheless, we hope that our unyielding focus on treatment personalization, our variety of programs and treatments, and our insistence on upfront clarity have set your mind at ease.
If you’re ready to take the first step toward a new life, free from addiction, you have found the drug rehab that accepts TRICARE you’ve been looking for in Harmony Ridge Recovery. Contact us today, and reclaim the life you deserve!
References:
https://www.tricare.mil/Plans/HealthPlans
https://www.tricare.mil/Plans/Eligibility
https://www.tricare.mil/Plans/Eligibility/DEERS
https://www.cdc.gov/nchs/nhis/health_insurance/hi_glossary.htm
https://www.tricare.mil/finddoctor
https://www.tricare.mil/costs/cost-terms
https://newsroom.tricare.mil/Articles/Article/3013179/10-tricare-health-care-terms-you-should-know
Jump To Section
Begin Your Journey to Healing Here
Ask me about recovery, I can help you!
Our recovery specialists are standing by 24/7 to help you or your loved one.
Or call us: 


