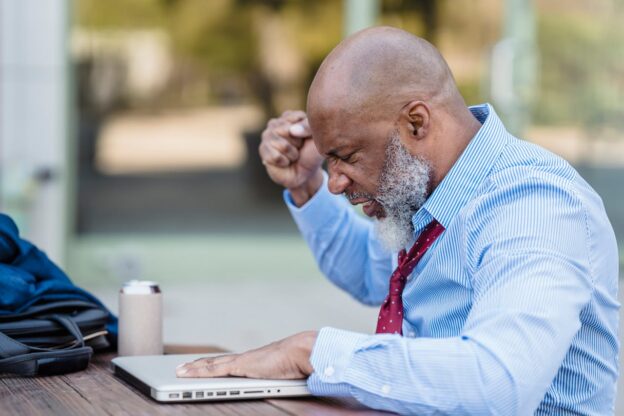
Alcohol can bring out a side of you that you might not recognize. For some, a personality change when drinking alcohol is noticeable, leading to unexpected moods or behaviors. Whether it’s becoming more talkative, aggressive, or emotional, alcohol affects everyone differently. These changes can be confusing, especially when they don’t reflect your usual personality. If you’ve noticed these shifts in yourself or someone else, it’s important to understand what might be happening. Sometimes, these changes are temporary, but for others, they can be part of a deeper issue. If alcohol is causing troubling personality shifts, addiction treatment centers in West Virginia can offer support. You don’t have to face this alone—there are solutions that can help restore balance and control.