Leaving the military changes almost everything about daily life. The structure, routine, and shared purpose disappear overnight, leaving many veterans feeling lost. The transition from military to civilian life often brings stress, confusion, and pressure to fit into a world that feels unfamiliar. Some turn to alcohol or drugs to cope, but that only adds new problems. You might feel isolated, struggle with mental health, or face challenges finding stable work. These struggles are real, and they can make recovery feel out of reach. You are not alone in this. Many veterans face the same issues, and support exists to help you through it. With the right guidance and care, it’s possible to manage stress in healthier ways and build a stable, fulfilling civilian life.
Understanding the Transition From Military to Civilian Life
The transition from military to civilian life often feels harder than expected. Veterans lose the structure and routine they relied on for years. Many feel unsure of their identity without the uniform and purpose service once gave them. Adjusting to civilian work, relationships, and culture can be overwhelming. Daily life looks completely different, and not everyone understands these struggles.

The transition from military to civilian life also brings emotional challenges like isolation and stress. These changes can trigger unhealthy coping habits if support isn’t available. Veterans may feel like they don’t belong in either world, which increases the risk of substance use. These difficulties explain why veterans struggle to seek rehab, even when treatment could help. That’s why the transition from military to civilian life requires specialized support and understanding. With the right help, veterans can rebuild a stable, fulfilling life.
Common Triggers for Substance Use in Veterans
The transition from military to civilian life can bring emotional pain, stress, and uncertainty. Veterans may turn to substances when overwhelmed, especially if support feels limited. Stress from adjusting to jobs, relationships, or health challenges makes coping harder. Many veterans say the loss of routine increases the pull toward alcohol or drugs. The transition from military to civilian life also leads to feelings of disconnection, which makes self-medication tempting. Some veterans even compare their struggles to those addressed in rehab for professionals, where stress and pressure often fuel addiction. Below are common triggers that veterans often face:
- PTSD symptoms: Flashbacks, nightmares, and anxiety push some toward substances.
- Chronic pain: Long-term injuries often lead to prescription misuse.
- Isolation: Lack of support increases loneliness and relapse risk.
- Employment stress: Difficulty finding stable work leads to frustration.
- Civilian adjustment: Struggles with daily routines encourage unhealthy coping.
Evidence-Based Treatment Options for Veterans
The difficult transition from military to civilian life can leave many veterans struggling with mental health and substance use. Adjusting to civilian life after military service often requires specialized treatment that addresses both visible and invisible wounds. Veterans benefit most when care is evidence-based, meaning proven therapies backed by research. These approaches focus on both mental health and addiction. Below are three methods that continue to show strong outcomes for those transitioning from military to civilian life.
Dual Diagnosis Treatment for PTSD and Addiction
Many veterans battle both mental health conditions and substance use at the same time. Dual diagnosis treatment gives them a way to address both together instead of separately. This matters because PTSD and addiction feed into one another, making recovery harder. Veterans dealing with trauma may use substances to cope, which worsens both problems.
With dual diagnosis treatment in West Virginia, veterans receive therapy that targets trauma while also supporting sobriety. This kind of care helps reduce relapse because it builds coping strategies and addresses root causes. For those facing the difficulty transitioning from military to civilian life, dual diagnosis programs provide hope. They recognize that healing from trauma and substance use must happen at the same time, not in separate steps.

Medication-Assisted Treatment (MAT) for Veterans
For veterans struggling with opioid or alcohol use, medication assisted treatment has become a trusted option. MAT uses FDA-approved medications like buprenorphine, methadone, or naltrexone along with therapy. These medicines reduce cravings, making it easier to stay focused on recovery. MAT is especially helpful for veterans who feel overwhelmed during the military transition to civilian life.
Many already face chronic pain or anxiety, which can lead to misuse of prescriptions. When paired with counseling, medication assisted treatment in West Virginia helps veterans stabilize their lives and reduce relapse risk. This combination treats both the physical side of addiction and the emotional challenges of adjusting to civilian life after military service. MAT doesn’t replace personal effort, but it gives veterans a stronger foundation to succeed in recovery.
Behavioral Therapies for Veterans
Counseling and behavioral therapy remain essential for long-term recovery. Approaches like motivational interviewing for substance abuse help veterans explore their own reasons for change. Instead of being told what to do, they learn to build motivation from within. This is important for anyone facing difficulty transitioning from military to civilian life, because self-direction builds confidence. Veterans often carry trauma and stress that shape their decisions.
Behavioral therapies help break negative patterns while teaching practical coping skills. Programs often include cognitive behavioral therapy, group counseling, and trauma-focused approaches. These tools give veterans healthier ways to manage stress without turning to alcohol or drugs. For those transitioning from military to civilian life, therapies like motivational interviewing for substance abuse create meaningful, lasting progress by connecting treatment directly to personal goals.

The Importance of Community and Peer Support
The veteran transition to civilian life often feels lonely, and many find themselves cut off from the sense of brotherhood that military service provides. This loss of connection can fuel substance use and depression. Strong community support plays a vital role in recovery because it replaces isolation with belonging. Veterans need spaces where they feel understood and valued. The following three areas highlight how peer support, family, and community organizations help those transitioning from military to civilian life.
Veteran Peer Support Programs
Peer support makes a big difference during recovery. Many veterans say the hardest part of the transition from military to civilian life is feeling alone. Being around others who truly understand your struggles can change everything. These connections replace isolation with belonging and encouragement. Veterans gain strength from shared experiences, and that support often helps them stay committed to recovery. Here are some ways peer support programs make a lasting impact:
- Shared experiences: Veterans connect with peers who faced the same struggles.
- Accountability partners: Encouragement to stay on track with recovery goals.
- Trust and understanding: Bonds that grow from military backgrounds and honesty.
- Hope through example: Seeing others succeed inspires continued effort.
- Guidance from peers: Practical advice from those adjusting to civilian life after military service.
Family Involvement in Recovery
Recovery works better when families stay involved. A strong support system at home provides encouragement and accountability. For those in rehab for veterans, family counseling often becomes part of the process. Loved ones learn about addiction, PTSD, and how to provide real support without judgment. This is especially valuable during the difficult transition from military to civilian life, when stress and disconnection can make recovery harder.
Families who stay engaged help reduce relapse risk and rebuild trust. The process isn’t always easy, but open communication makes a difference. Veterans adjusting to civilian life after military service benefit greatly when those closest to them understand what they’re going through. Rehab for veterans that includes families creates a more stable environment and increases long-term success in recovery.

Community Resources and Organizations
Local organizations and rehabs in WV play a major role in supporting veterans after treatment. These resources provide everything from housing help to job training, giving veterans stability outside of therapy. For those facing difficulty transitioning from military to civilian life, this kind of support can mean the difference between progress and relapse. Community programs also create opportunities for veterans to build new friendships, find purpose, and give back.
Many centers specifically focus on veterans, which helps ease the adjustment to civilian life after military service. The sense of belonging offered by rehabs and related programs reduces isolation. Veterans learn that they aren’t alone, and they discover places where help is always available. Community support ensures recovery continues well beyond initial treatment.
The Role of PTSD and Trauma in Substance Use
PTSD affects many veterans, and its impact often grows during the transition from military to civilian life. Flashbacks, nightmares, and hypervigilance make daily living difficult. Some veterans use alcohol or drugs to escape these feelings, but that only creates new problems. Trauma doesn’t disappear after service ends. In fact, it often becomes more intense without the military structure.
The transition from military to civilian life highlights unresolved wounds, and self-medication becomes a common response. Substance use may seem like short-term relief, but it increases anxiety and depression in the long run. Many veterans find themselves caught between trauma and addiction, each making the other worse. The transition from military to civilian life is when many realize they need real help to manage PTSD and build lasting recovery.

Social and Cultural Barriers in Civilian Reintegration
The transition from military to civilian life can feel isolating, especially when cultural differences create distance. Veterans often say civilians don’t fully understand their experiences. Stigma around addiction and mental health makes it harder to ask for help. Many veterans avoid treatment because they fear judgment. The transition from military to civilian life also removes the strong support of unit culture, leaving some veterans without trusted connections. Below are common barriers veterans face when reintegrating:
- Stigma: Fear of being labeled stops veterans from seeking help.
- Civilian culture shock: Daily life feels unfamiliar and confusing.
- Lack of community: Veterans lose the sense of belonging from service.
- Misunderstanding: Civilians may not grasp military trauma.
- Limited resources: Access to veteran-focused care is uneven.
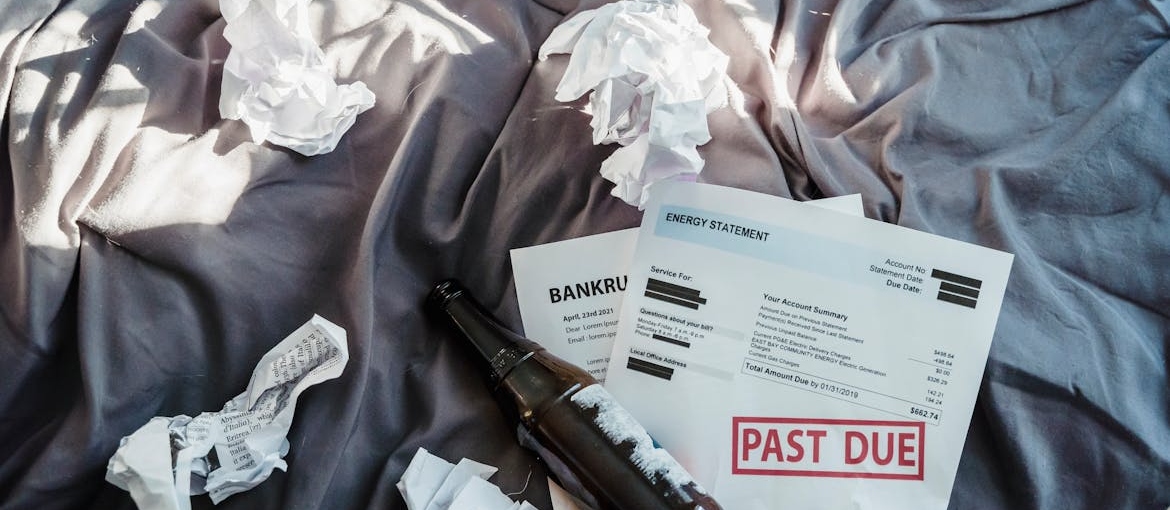
Financial Stress and Its Impact on Recovery
Money problems often add pressure during the transition from military to civilian life. Veterans may leave service with limited savings, medical expenses, or difficulty finding steady work. Financial stress can push some toward alcohol or drugs as a way to escape the anxiety. The difficulty transitioning from military to civilian life becomes even harder when bills pile up or housing feels uncertain.
Addiction can worsen these struggles, leading to job loss and more instability. Veterans who enter a drug rehab that accepts Tricare can often find relief, since insurance helps cover the cost of care. Financial counseling during treatment also teaches veterans how to manage money, set goals, and access benefits. Addressing finances alongside mental health and addiction builds a stronger foundation for adjusting to civilian life.
Building a Healthy Civilian Lifestyle After Service
Recovery improves when veterans create new routines that bring stability and purpose. The transition from military to civilian life can feel empty without the structure once provided by service. Developing healthier habits helps fill that gap. Veterans who focus on fitness, employment, and community connection often report stronger recovery outcomes. The transition from military to civilian life doesn’t have to lead to isolation. Instead, it can become a chance to build a new, balanced life. Below are ways veterans can create a healthier civilian lifestyle:
- Daily exercise: Movement helps reduce stress and improve mood.
- Balanced meals: Nutrition supports energy and recovery.
- Job training: Skills programs provide purpose and stability.
- Social groups: New friendships replace isolation.
- Volunteering: Helping others rebuilds confidence and connection.
Taking the First Step Toward Healing
The transition from military to civilian life can feel overwhelming, and it’s normal to struggle. Losing structure, facing new expectations, and carrying invisible wounds can push many veterans toward unhealthy coping methods. If you’ve turned to alcohol or drugs, it doesn’t mean you’ve failed. It means you need support. Recovery is possible, and treatment can help you build the tools to manage stress and heal from trauma. You don’t have to face this alone—there are programs built for veterans that understand your challenges and provide real solutions. Reaching out for help is a step toward a healthier future, not a sign of weakness. With the right support, you can find stability, rebuild purpose, and create a civilian life that feels meaningful again.



